A University of Houston (UH) vision scientist has received a $1.85 million grant from
the National Institutes of Health (NIH) to investigate whether his techniques are
more effective than others in understanding the earliest changes of glaucoma, which
could lead to developing a way to earlier diagnose this potentially blinding disease.
Jason Porter, an assistant professor of vision science and biomedical engineering,
uses a state-of-the-art instrument that takes sharper, higher-resolution images of
the eye than current clinical instruments. The adaptive optics scanning laser ophthalmoscope,
or AOSLO, device Porter uses corrects for the eye’s optical imperfections and captures
high-resolution movies on a cellular-level in the living eye. Since 2009, his team
has been using the AOSLO to image normal and diseased eyes, and the instrument has
become a key component of their work in glaucoma, with the goal of using it to better
understand retinal diseases.
“Even when wearing glasses or contact lenses, our eyes still have subtle optical imperfections,
and these imperfections limit the ability of current clinical instruments to obtain
high-resolution images in the eye on a cellular-level,” Porter said. “The AOSLO uses
a technology called adaptive optics to correct for these subtle imperfections, thereby
improving the eye’s optical quality and allowing our instrument to capture sharp images
of single cells in living eyes. This could potentially lead to more sensitive imaging
techniques that may better clarify the causes of glaucoma.”
The knowledge resulting from this research, Porter explains, will enhance clinicians’
understanding of the development and progression of glaucoma and may provide earlier
recognition of structural damage from the disease. The study’s results also may result
in more sensitive, improved imaging diagnostics used by optometrists and ophthalmologists
to prevent vision loss by earlier detecting structural damage to the retina and optic
nerve head, as well as help eye doctors to better evaluate and track the effectiveness
of glaucoma treatments.
Porter’s work concentrates on examining the lamina cribrosa, which is the sponge-like,
porous part of the eye in the optic nerve head that provides structural and functional
support to the retinal axons as they exit the eye and move to the brain. Signals detected
by the retina are transmitted through retinal axons that exit the eye through the
optic nerve head and tend to travel in bundles, weaving their way through the pores
in the lamina cribrosa and exiting the eye to go to the brain. 
“While my lab has expertise in high-resolution imaging of the eye and the lamina,
we provide only one piece of the puzzle in glaucoma,” Porter said. “It is very important
that we relate the changes we see in our images of the lamina cribrosa with other
changes that occur in the retina and in a patient’s vision. Therefore, our work is
really a collaborative effort between several scientists and clinicians in the College
of Optometry.”
Porter’s group works closely with Ronald Harwerth, John and Rebecca Moores Professor
and chair of the department of basic sciences, who is a leading expert in how structural
changes in the optic nerve head and retina are related to vision loss in glaucoma.
They also work in partnership with Laura Frishman, John and Rebecca Moores Professor
and associate dean for graduate research, who is a leading expert in the functional
changes in vision that occur in the retina and visual pathways in glaucoma, as well
as other optic neuropathies. As the study progresses, Porter’s team also will collaborate
with Danica Marrelli, a clinical professor and optometric glaucoma specialist, who
will help recruit normal and glaucomatous patients, as well as interpret the clinical
data acquired in these eyes.
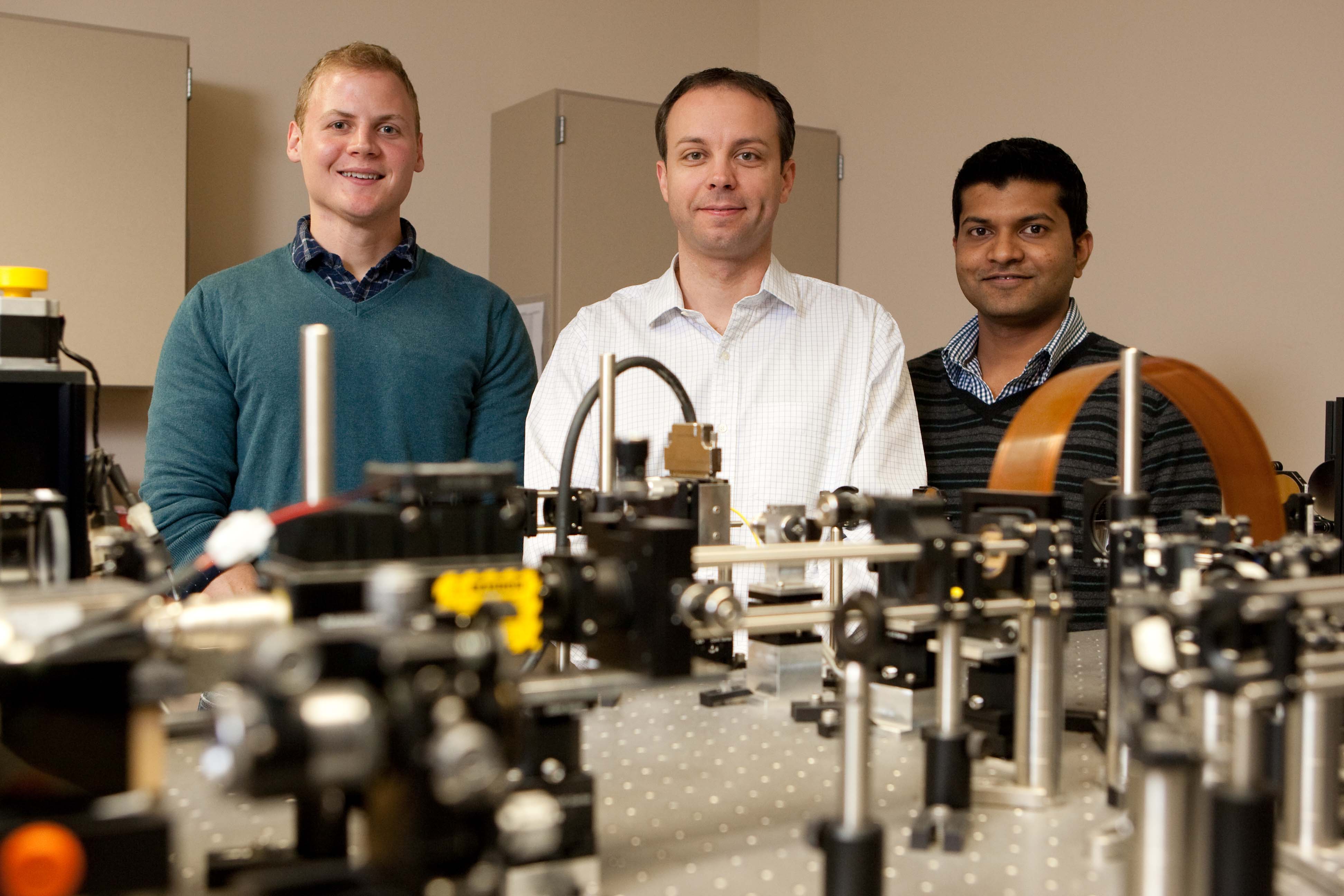
Working directly with Porter on lamina cribrosa imaging are two of his graduate students.
Kevin Ivers is a Ph.D. candidate in the College of Optometry’s vision science and
physiological optics graduate program and has developed a great deal of the methodology
for imaging the lamina cribrosa using the AOSLO. Nripun Sredar, a Ph.D. computer science
student and jointly advised by Porter and professor George Zouridakis in the College
of Technology, is developing methods to model the lamina cribrosa in 3-D to improve
their understanding of how the lamina pores may change with disease progression.
###
Editorial Note: High-resolution photos of Jason Porter in his lab are available to
media by contacting Lisa Merkl.
About the University of Houston
The University of Houston is a Carnegie-designated Tier One public research university
recognized by The Princeton Review as one of the nation’s best colleges for undergraduate
education. UH serves the globally competitive Houston and Gulf Coast Region by providing
world-class faculty, experiential learning and strategic industry partnerships. Located
in the nation’s fourth-largest city, UH serves more than 38,500 students in the most
ethnically and culturally diverse region in the country.
About the UH College of Optometry
Since 1952, the University of Houston College of Optometry (UHCO) has educated and
trained optometrists to provide the highest quality vision care. One of only 20 optometry
schools in the country, UHCO offers a variety of degree programs, including Doctor
of Optometry (O.D.), a combined Doctor of Optometry/Doctor of Philosophy (O.D./Ph.D.),
Master of Science (M.S.) and Doctor of Philosophy (Ph.D.). UHCO serves an average
of 36,000 patients a year through The University Eye Institute and its satellite clinics.
For more information about UH, visit the university’s Newsroom.
To receive UH science news via e-mail, sign up for UH-SciNews.
For additional news alerts about UH, follow us on Facebook and Twitter.