Research News
Improving Adherence, Outcomes
Aparasu's Work to Assess Multiple Sclerosis Patient Medication Adherence, Relapse Rates Receives AHRQ Support
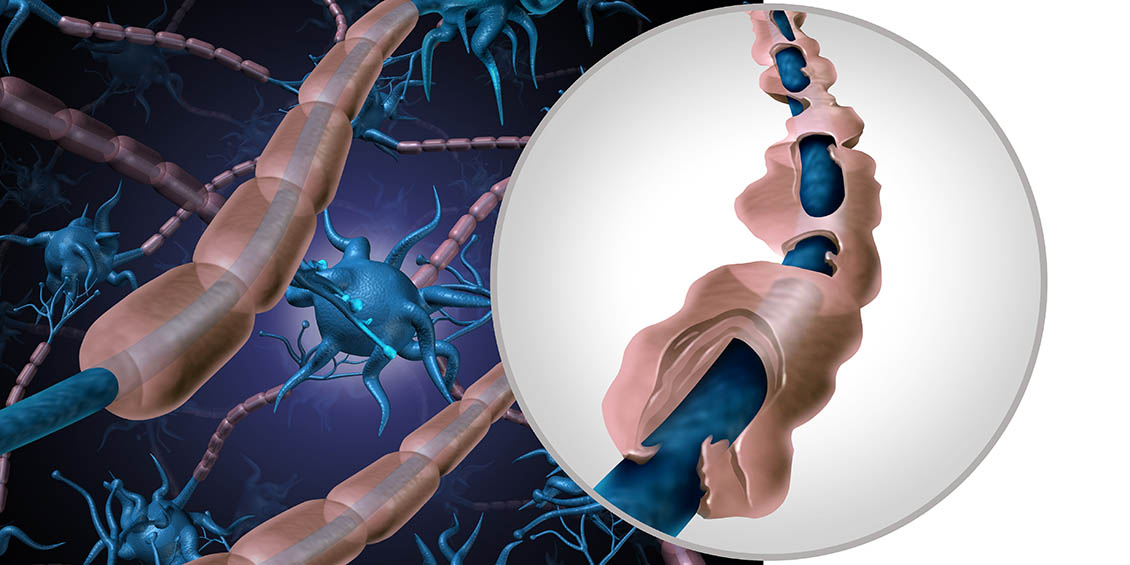
November 29 — UH College of Pharmacy's Rajender R. Aparasu, Ph.D., FAPhA, Sanober & Mustafa Lokhandwala Endowed Professor of Pharmaceutical Health Outcomes and Policy, is taking a new approach to better understand how patients with multiple sclerosis (MS) are adhering to their medication therapy.
Aparasu is specifically investigating MS patients' adherence to their oral disease modifying agent (DMA) regimen using a statistical method known as group-based trajectory modeling (GBTM). With GBTM, individuals are classified into groups based on their prescription-filling pattern over time. This investigation will specifically evaluate the outcomes of these trajectories, including relapse rates involving inpatient hospitalization or an outpatient visit with a corticosteroid prescription within 30 days.
 Aparasu's research will focus on the three oral DMAs for MS first introduced: fingolimod, teriflunomide, and dimethyl fumarate. Although oral DMAs offer greater convenience for patients, the medications differ in their treatment regimens — including the number of pills taken in a day, which may also change after a given time period. These differences can impact adherence and, consequently, outcomes such as relapse rates.
Aparasu's research will focus on the three oral DMAs for MS first introduced: fingolimod, teriflunomide, and dimethyl fumarate. Although oral DMAs offer greater convenience for patients, the medications differ in their treatment regimens — including the number of pills taken in a day, which may also change after a given time period. These differences can impact adherence and, consequently, outcomes such as relapse rates.
"Group-based trajectory modeling provides a more accurate picture of adherence patterns over time than more traditional methods of measuring adherence based on refill records or claims in which adherence is assessed as a single value," Aparasu said. "Limitations of these traditional methodologies, such as medication possession ratio (MPR) and proportion of days covered (PDC), include failure to account for time-related changes in adherence.
"With trajectory modeling, patients are classified into different adherent trajectory groups such as complete adherers and slow and rapid discontinuers based on the prescription-filling pattern over time, with each trajectory representing a distinct adherence pattern."
"Overall, the aim is to inform clinicians and patients regarding treatment decisions with regard to the use and adherence to oral DMAs, and ultimately to improve health outcomes," Aparasu said.
The project evaluating dynamic medication adherence patterns over time and its impact on clinical outcomes in MS is supported by a one-year, $100,000 grant from the Agency for Healthcare Research and Quality.