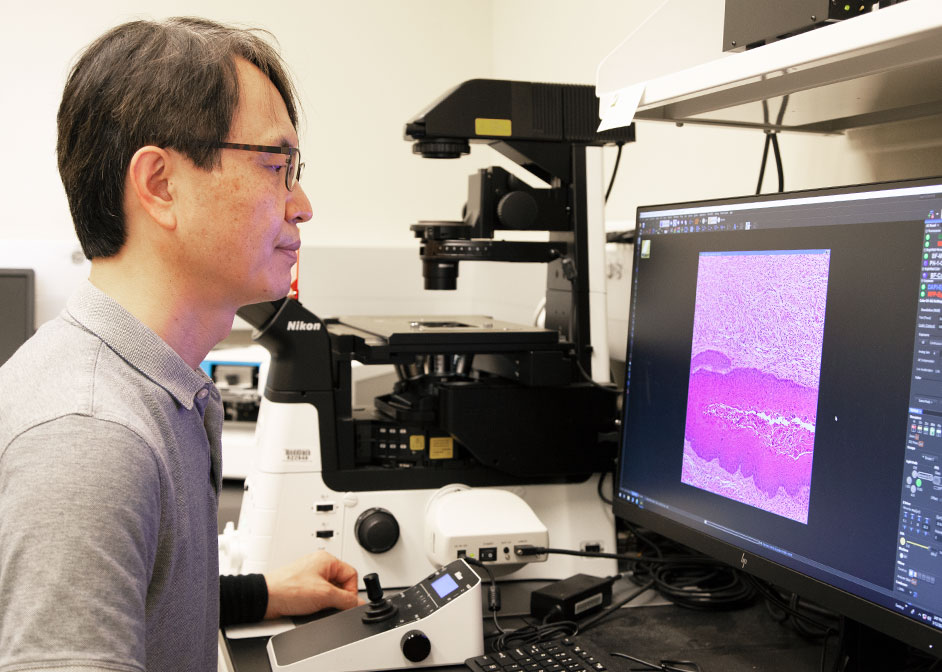
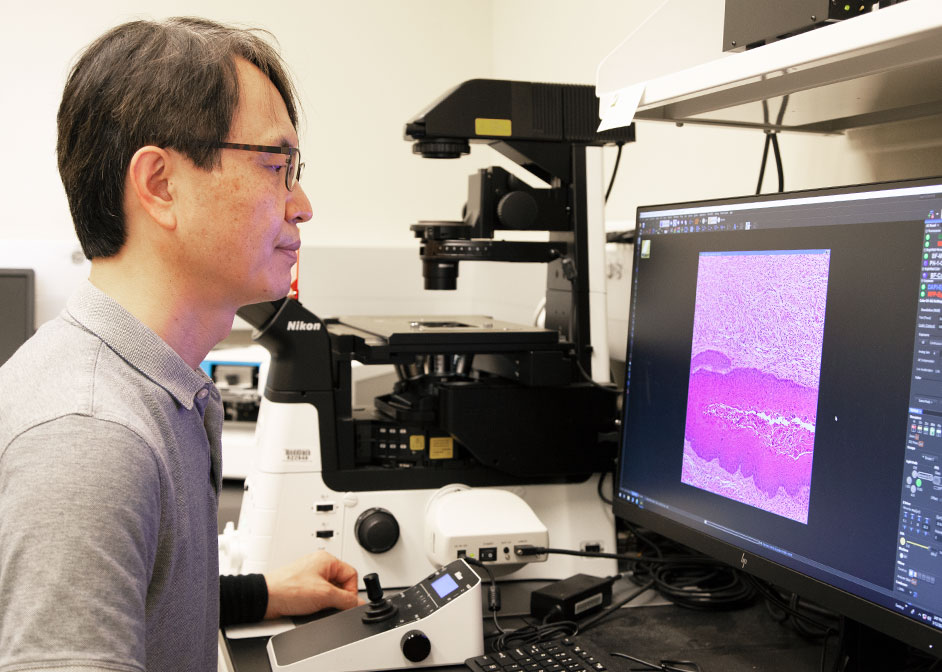
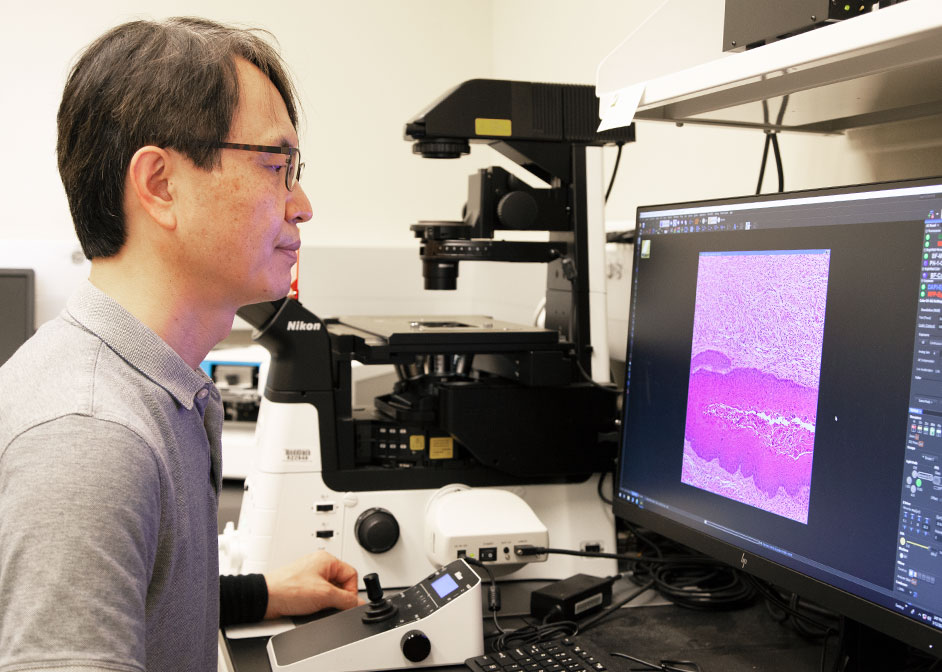
- 04/12/2021 01:00:00 AMCNRCS Researchers Find Connection Between Progesterone Receptor and Cervical CancerSanghyuk Chung and graduate student led study published in Molecular Cancer Research journal.https://mcr.aacrjournals.org/content/19/1/42
 Biology & Biochemistry
Biology & Biochemistry